Abstract
Introduction:
We previously demonstrated Black patients with acute myeloid leukemia (AML) are more likely to require ICU-level resources at initial presentation. This disparity in acuity at presentation explained 62% of the two-fold racial disparity in early mortality (Winestone Am J Hematol 2017). We sought to expand these findings using a more detailed data source that leverages electronic medical record (EMR) data from two large institutions. We hypothesized that disparities in severity at presentation by race, ethnicity, and socioeconomic status would be identified in granular EMR data for children with acute lymphoblastic leukemia (ALL) and AML.
Methods:
Acute leukemia patients who were diagnosed at Children's Hospital of Philadelphia or Texas Children's Hospital (2006-2014) were included. Patients who transferred from a referring hospital or whose race was specified as Asian, other, or unknown were excluded. Race and ethnicity were combined into 3 mutually exclusive categories: Hispanic, non-Hispanic White, and non-Hispanic Black. The first set of vital signs (blood pressure, heart rate, respiratory rate, and temperature) and the timing of key diagnostic evaluations were manually abstracted. Patient age, sex, race/ethnicity, residential address, and results of selected laboratory tests from the first 72 hours after admission underwent automated extraction from the EMR. Residential addresses were batch-matched to geo-coordinates linking each patient to a census-derived block group. The following measures of socioeconomic status (SES) were evaluated: median household income, education, unemployment, and crowding. Vital signs were interpreted using age-specific American Heart Association reference ranges. Individual and composite lab-based definitions created a priori were used to identify high disease burden, risk of infection, renal dysfunction, abnormal coagulation (prothrombin time >17 or fibrinogen <100) and liver function (AST/ALT>200 or bilirubin >2.5 or GGT>150). Log-binomial regression was used to compute unadjusted prevalence ratios (PR) and corresponding 95% confidence intervals (CI) comparing incidence of vital sign and laboratory abnormalities by race/ethnicity and block group SES. Stratification by leukemia type (AML vs. ALL) allowed for assessment of heterogeneity in associations of interest. Covariates that were associated with race and thus were potential confounders were also included in multivariable models to obtain adjusted PRs.
Results:
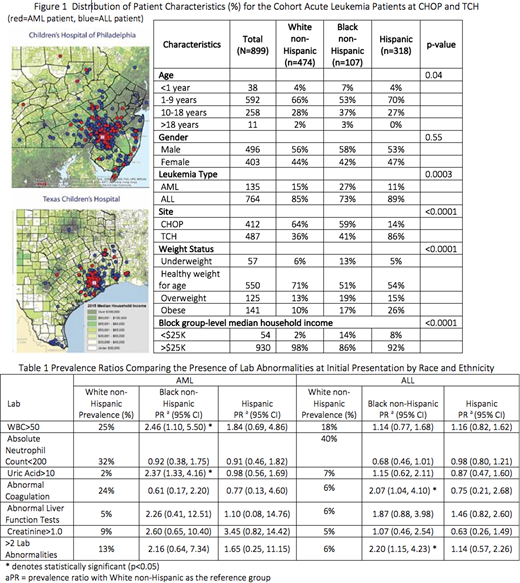
A total of 899 acute leukemia patients (474 non-Hispanic White, 318 Hispanic, and 107 non-Hispanic Black) were included. Figure 1 shows patient characteristics including patients' geo-coordinates mapped onto census block group median household income. Vital signs at presentation were generally similar across racial/ethnic groups with the exception of heart rate among Hispanic patients (62% vs. 53%, p=0.03). Black patients with AML had an increased prevalence of elevated white blood cell (WBC) count and uric acid and Black patients with ALL demonstrated increased prevalence of coagulopathy compared to White non-Hispanic patients (Table 1). For both AML and ALL, Black patients were more likely to have more than 2 lab abnormalities relative to White non-Hispanic patients. There were no clinically significant differences in time to key diagnostic evaluations by race/ethnicity; median time to CBC was under 2 hours for all racial/ethnic groups, median times to bone marrow biopsy and lumbar puncture ranged from 25-39 hours, and median time to chemotherapy was between 2-3 days. None of the measures of SES were significantly associated with abnormal vital signs, abnormal labs, or prolonged time to key diagnostic evaluations.
Conclusions:
Black patients with newly diagnosed AML present with increased prevalence of high disease burden as evidenced by elevated WBC and uric acid. Across acute leukemia types, Black patients are more likely to present with more than 2 lab abnormalities; these lab abnormalities likely represent physiologic dysfunction at diagnosis and may compound one another to explain the previously observed racial disparity in ICU-level care requirement. Similar ethnic differences were not observed among Hispanic patients with AML or ALL. We are conducting ongoing investigation into the impact that rurality and distance to the hospital have on initial presentation.
Fisher:Merck: Research Funding; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.